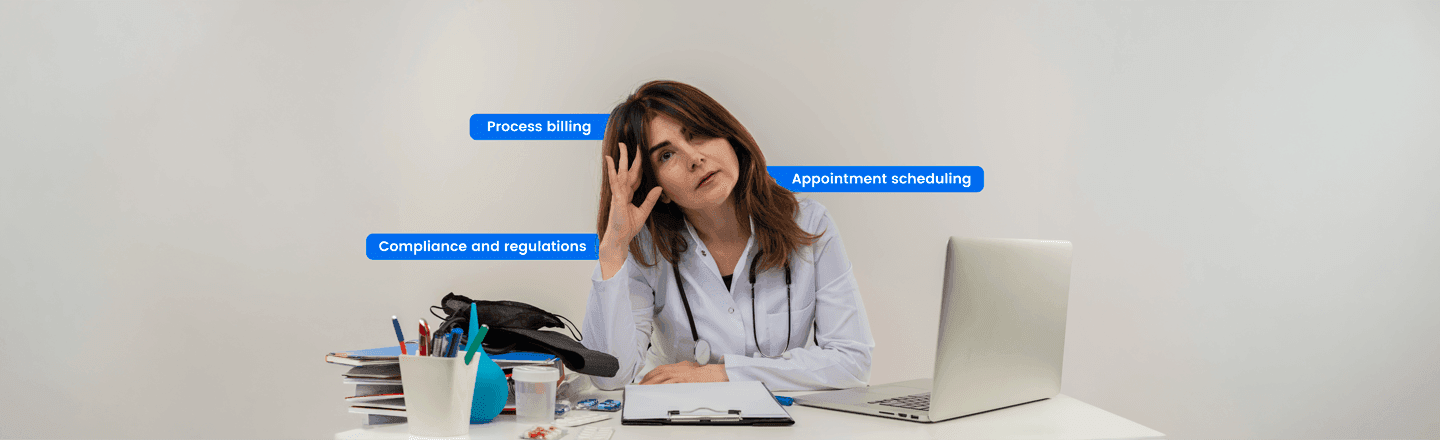
Walk into almost any clinic these days, and the first thing you will notice is the clinical staff busy doing paperwork instead of focusing on their patients. Consequences? Burnout staff, frustrated patients, and lost clinical revenue that clinics cannot afford to miss. Longer wait times can lead to rushed visits and risk errors in their care.
It’s not only a workflow problem. It also affects the staff morale and patient trust.
To have more focus on patients, healthcare departments can hire specific healthcare roles. For example, medical assistants or receptionists by using EHR systems properly.
What is Administrative Burden in Healthcare
Administrative burden in healthcare happens when doctors and clinical staff spend most of their time on non-clinical tasks. These tasks include charting, insurance verification, data entry, scheduling appointments, billing, compliance, and communicating with insurance providers.
A primary physician seeing 25 patients a day would approximately spend 15 minutes per session. An additional 10 minutes are needed to make notes post-appointment, and they might not be able to do so after every appointment, as there are multiple fields to check through. It can easily result in a lack of properly organized notes and charts that a doctor will need for a follow-up session.
The Most Time-Taking Tasks for Doctors & Nurses
Here is where most of the time goes, actually:
Documentation and charting
Accurate documentation is essential for any clinic. It involves recording patient visits, updating medical records, and following EHR (electronic health records) requirements. From dealing with patient data safety to legal compliance, most of the responsibility falls on the staff.
Patient communication
Doctors or physicians see a lot of patients in a day, making it harder to communicate with them the way they want to.
They might not be able to answer their urgent queries if asked via an email or a phone call, as long as they are buried in documenting every detail. Therefore, slow or a lack of patient communication can affect their retention rate.
Entering data into multiple systems
Many healthcare facilities use multiple systems for data entry. For example, EHR documentation, Billing and revenue cycle management, and more. This duplicate data entry on multiple platforms increases the risk of errors and burden on staff.
Scheduling and follow-ups
Appointment management is another time-consuming task for clinicians. When doctors have to coordinate schedules, confirm appointments and manage cancellations, it takes them away from patient care. Therefore, specialized role allocation can solve this problem, and doctors can have a focused approach towards their patients.
Revenue cycle management
Clinicians and administrative staff spend most of their time on coding and submitting accurate claims. They also promptly address claim denials to avoid delays in reimbursement.
Mismanagement of the revenue cycle (RCM) can lead to delayed payments, lost revenue, and additional administrative strain on clinical teams. To reduce this burden, healthcare practices can hire dedicated billing specialists.
Manual Work Hours Spent by Specialties for Administrative Tasks
According to the Medscape Physician Compensation Report 2023, a healthcare practitioner spends an average of 15 hours per week on administrative work, including documentation.
To better comprehend the burden of paperwork, let’s take a closer look at the number of hours spent on administrative work.
| Healthcare Specialty | Hours Spent on Documentation |
| Physical Medicine | 19 hours |
| Internal Medicine | 18 hours |
| Family Medicine | 17 hours |
| Cardiology, Endocrinology | 16 hours |
| Pediatrics, General Surgery | 15 hours |
| Orthopedics | 14 hours |
| Emergency Medicine, Gastroenterology | 13 hours |
| Dermatology, Plastic Surgery | 11 hours |
| Ophthalmology | 10 hours |
How the Administrative Burden in Healthcare Impacts Providers, Staffers, & Revenue
Administrative overload impacts providers, staffers, and revenue in many ways:
Provider impact
Burnout: When doctors spend a major portion of their time managing records. Burnout is real that leads to inefficiency in work.
Reduced job satisfaction: Provider time spent on paperwork disengages them from their core duties of seeing patients and increases turnover risk.
Lower productivity: Time spent on non-clinical tasks reduces the clinical productivity of providers.
Patient impact
Longer wait times: Patients wait longer when clinicians are busy with paperwork.
Rushed visits: Patients don’t feel good when doctors see a huge volume of patients in a short span of time. It can lead to missed important details, such as past illness reports, that can cause errors in prescriptions.
Documentation errors: Non-clinical workload in hospitals can cause documentation errors when clinical staff have other tasks to do.
Financial impact
Lost billable hours: Time spent on paperwork is time you can’t bill for. When staff spend most of their time on non-billable tasks, they miss their important billable hours.
Increased overtime costs: Hospitals pay overtime costs to their staff to manage the workload, which is a strain on their revenue.
Claim denials and delayed reimbursement: In healthcare, insurance claims may be denied due to errors in documentation or coding issues.
How Patients are Affected (The Part Clinic Often Misses)
Administrative burden does not harm staff only; it also has a bad impact on patients. For example, long wait times for appointments are growing concerns. According to a survey by Merritt Hawkins, the average time for appointments in US metropolitan areas has increased to 26 days.
The survey shows that insurance verifications and all other paperwork are major contributors to this delay. Rushed visits can compromise care quality, and this burden can increase the chances of errors in records and billing.
Practical Ways Healthcare Practices are Reducing Administrative Load
Clinics are reconsidering how to handle documentation and adopting new strategies to overcome this burden.
Workflow restructuring
Separation between administrative roles and clinical roles is the best solution to restructure workflow in a better way.
Clinicians are encouraged to focus on patient care and treatment planning, while other administrative roles, such as billing and insurance policy, should be handled by administrative staff.
Many healthcare facilities conduct workflow audits to identify issues. By redesigning task allocation and clarifying accountability, documentation errors and long patient waiting times can be minimized.
Documentation delegation
Healthcare facilities are introducing medical scribes, documentation specialists, and support roles to reduce administrative load. Medical scribes ensure accurate record-keeping and let doctors spend more time with their patients rather than handling paperwork.
The result? Fewer errors, patient satisfaction improves, clinicians are happy, and they can see patients without extending working hours.
Automation and digital integration
Modern electronic platforms such as EHR, Epic, and Cerner can make everyday clinic work a lot easier. Instead of staff sending every detail manually, these automation tools can send appointment reminders, refill prescriptions, and automatically track compliance.
When everything is connected properly, there are fewer chances of data duplication, and it increases accuracy.
Role redistribution and remote support
Many healthcare providers are shifting towards hiring remote staffing, which costs less and reduces the burden on clinicians.
Virtual assistants and remote administrative professionals manage tasks such as insurance follow-ups, documentation processing, patient communications, and data entry.
Healthcare facilities do not need to extend their space, as these tasks do not need a desk in the clinic. They can be operational remotely. When admin tasks are handled separately, doctors can fully focus on their patients.
How Healthcare Practices are Reducing Administrative Costs with Remote Staffing
Handling tasks like medical billing, revenue cycle management, and patient follow-ups can take hours that physicians can instead spend on their patients.
Therefore, instead of traditionally hiring an in-house assistant, many healthcare practices are onboarding virtual assistants for administrative tasks. They organize billing and coding, prior authorizations, verifies insurance documents, among other major tasks.
Not only does this help to reduce the documentation load on in-house staff and doctors, but it also makes the workflows efficient as all details are streamlined into the EHRs.
That’s how one of the healthcare practices, Glenwood Medical Association, streamlined its revenue by hiring remote billing assistants. They were able to save $ 35,000 annually (which is impressive).
It proves that remotely hiring people to get the job done might be one of the most cost-effective strategies.
Let’s Take the Admin Stress Off Your Shoulders
Administrative burden in healthcare doesn’t slow down your clinic. Lack of right-skilled talent does.
A remote staffing company like Remote Scouts helps clinics onboard HIPAA-trained, HIPAA-aligned virtual assistants who handle medical billing, revenue cycle management, and other administrative tasks, freeing clinicians to spend more time with their patients.
Healthcare practices can reclaim lost time and nurture their patient’s experience by focusing on them and delegating the documents and notes to the virtual assistant.
Free your team from clerical workload and let them focus on what they do best, i.e., healing patients.
Most Frequently Asked Questions
Which U.S. businesses benefit the most from nearshore VA?
Nearshore virtual assistants are ideal for a wide range of founders and entrepreneurs, professional services like medical, legal, and financial, growing SMBs, and large enterprises managing multi-departments and cross-team communications.